Pro and con for systematic screening for prostate cancer in Denmark - a review article
Signe Benzon Larsen1-3 & Andreas Røder1, 4
Systematic PSA-based screening for prostate cancer remains controversial due to the trade-off between reduced mortality and risk of overdiagnosis and overtreatment. Adding new tools like magnetic-resonance-imaging-targeted biopsies and genetic markers may limit the harms, but we lack definitive mortality data. While opportunistic PSA testing is widely used in Denmark, unsystematic use may potentially be harmful. Introduction of a systematic screening programme in Denmark requires careful consideration of the clinical, psychological, societal and economic impacts, and Danish politicians should thus engage in the debate to clarify these issues.
PSA-based screening reduces prostate cancer mortality but causes considerable overdiagnosis and overtreatment.
Risk-stratified screening and magnetic-resonance-imaging-targeted biopsies may reduce harms, but long-term mortality data remain lacking.
Opportunistic PSA testing is widespread in Denmark and potentially harmful.
Introduction of a screening programme requires careful healthcare policy consideration.
Whether or not to implement systematic screening for prostate cancer has generated ongoing debate since the 1980s, with experts, patient organisations and policymakers weighing the potential benefits of early detection against the risks of overdiagnosis and unnecessary treatment. As one of the leading causes of cancer-related mortality among men worldwide, the search for effective strategies of early detection has made prostate cancer one of the most diagnosed cancers globally. This is also the case in Denmark, where 4,600 men are diagnosed annually and around 1300 die of the disease. The increasing incidence has been driven by the use of the blood-based biomarker prostate-specific antigen (PSA) [1, 2]. PSA is an eminent biomarker to identify men with prostate cancer and is currently the best tool for systematic screening. Although regular PSA testing in the 50-70-year age range may reduce prostate cancer mortality, harms caused by overdiagnosis and overtreatment keep triggering the debate on the pros and cons of introducing systematic PSA-based screening [2, 3]. In recent years, we have experienced increasing political lobbying to introduce screening in Europe and Denmark, sparked by the EU Commission's Beating Cancer Plan 2023 that advocates an increased focus on early detection of prostate cancer in Europe.
In this paper, we evaluate the key controversies in systematic screening for prostate cancer and discuss the potential implications of implementing a national PSA-based screening programme in Denmark.
Current evidence of PSA-based screening
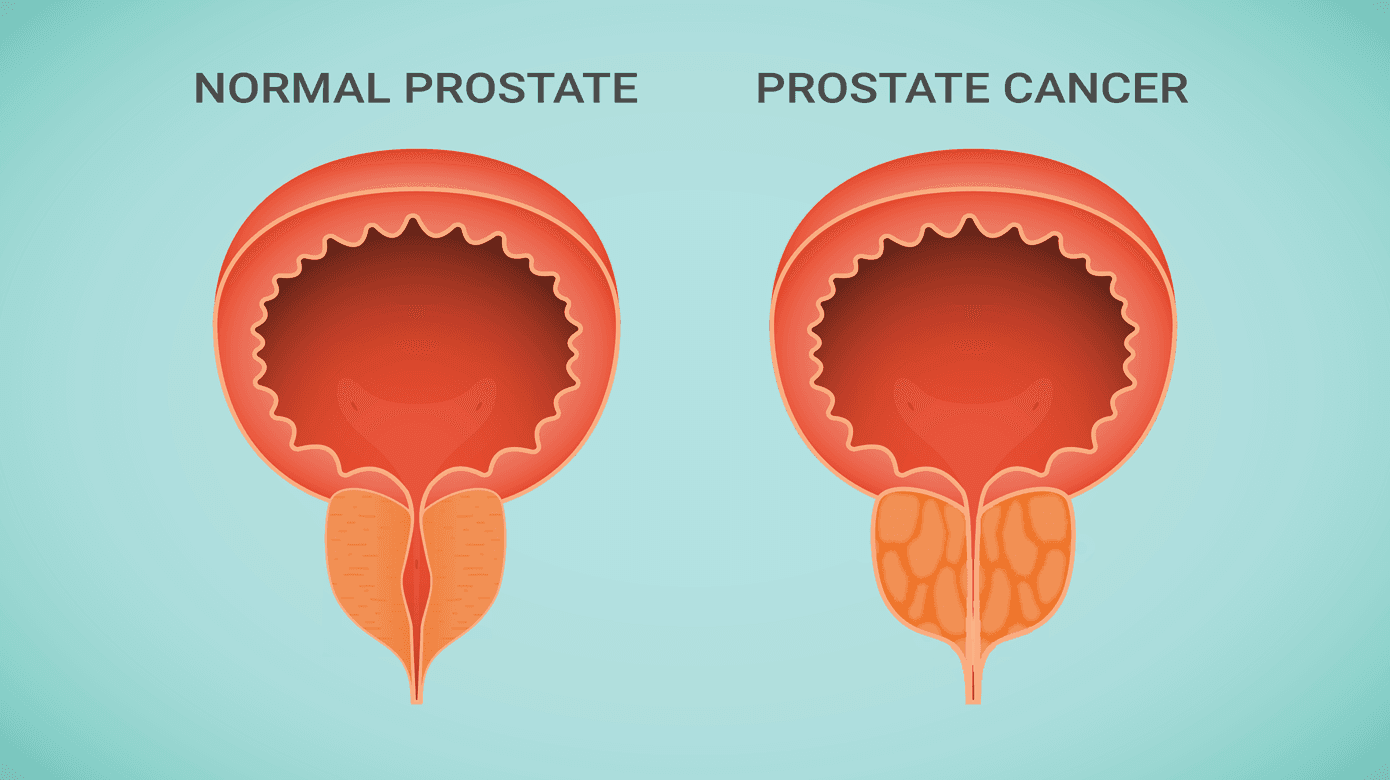
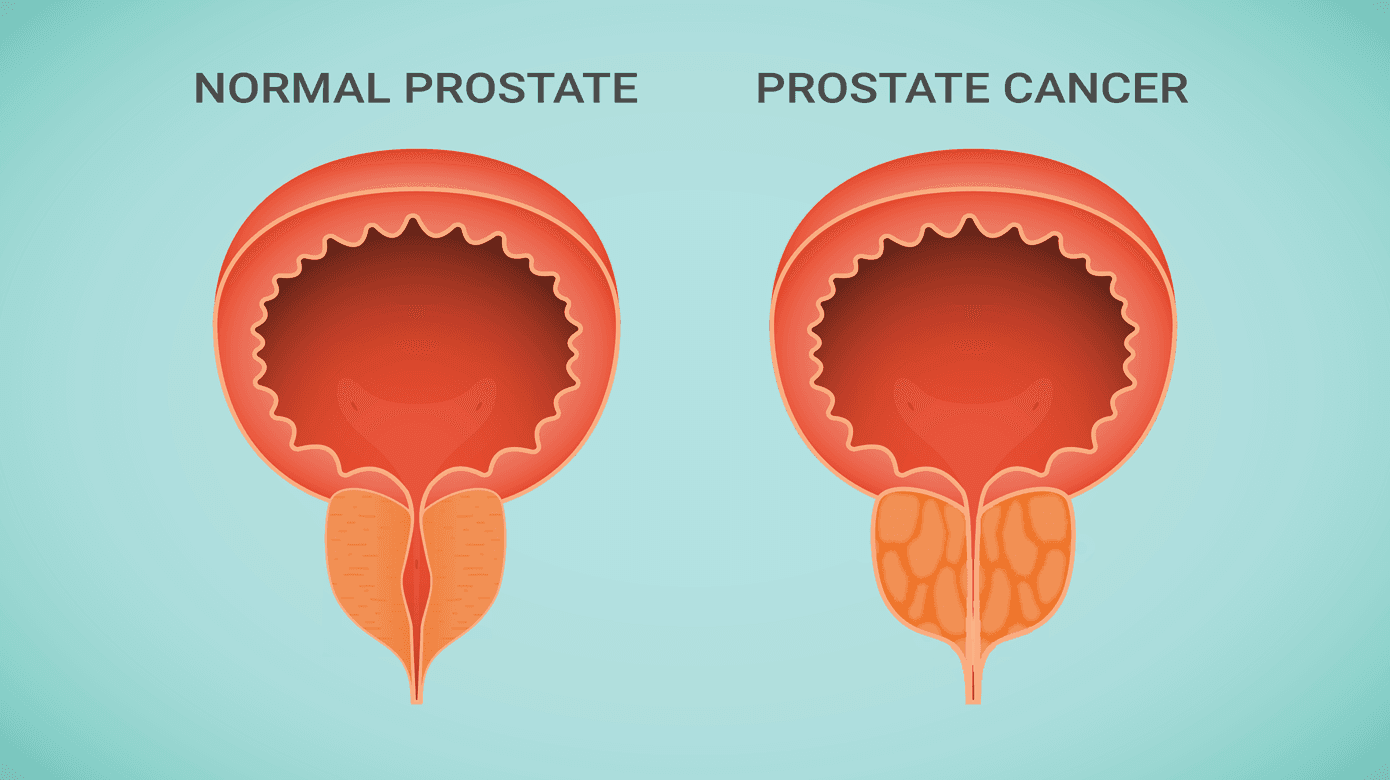
A decision to implement systematic screening should be based exclusively on the advances for the total male population and the healthcare system. Extensive clinical research has investigated various systematic approaches to early prostate cancer detection, most relying on PSA measurements [2, 4, 5]. Although the PSA test is not cancer-specific. it is excellent for establishing prostate cancer, including non-aggressive cancers. Large-scale studies suggest that systematic PSA-based screening reduces prostate cancer-specific mortality, but raise concerns about overdiagnosis and overtreatment that continue to challenge the overall trade-off between benefits and harms [3].
In 1994, the large European randomised study of screening for prostate cancer (ERSPC) was initiated to investigate the effect of PSA-based screening on prostate cancer mortality [6]. The study included men from several European countries with varying age spans, screening intervals and PSA thresholds between the study centres [7, 8]. In the latest publication, including a 16-year follow-up, the relative reduction in prostate cancer mortality was 20% between men in the screening and control arm [3]. To avoid one man dying of prostate cancer, 570 needed to be invited (NNI), and 18 needed to be diagnosed, indicating considerable overdiagnosis. Overdiagnosis covers cancer diagnoses detected by screening that would not have caused symptoms or death during the lifetime of a man and remains the most challenging impediment to the success of systematic prostate cancer screening. Depending on the calculation method used, overdiagnosis fell in the 40-50% range in the ERSPC trial, with the highest rates being observed in the two screening centres showing statistically significant reductions in prostate cancer mortality [9]. Currently, the findings from the ERSPC comprise some of the best evidence on PSA-based screening [2].
Risk-stratified screening
An obvious way to minimise overdiagnosis is individual risk-stratified screening, which may further lower the number needed to screen, reduce biopsies and overtreatment, and reduce expenses for subsequent treatment [10, 11]. But adding tests and examinations may complicate a screening programme, thereby increasing the expenses and reducing participation. We are, however, far from knowing how to stratify men to optimise the screening procedures, and no studies have yet provided evidence on cancer-specific mortality, which should be the ultimate endpoint.
Some randomised clinical trials using different risk-stratified approaches have been initiated in recent years [12–15]. Although these studies are ongoing, and the main findings have therefore yet to be reported. Some preliminary findings regarding participation, biopsy and cancer detection rates have been published. Screening procedures differ substantially across the studies, with variations in age, screening intervals, PSA thresholds, use of additional biological markers (e.g., molecular sub-forms of PSA, human kallikrein-related peptidase 2 (hK2), PSA density), biopsy strategies (e.g., number of cores, systematic versus magnetic resonance imaging (MRI)-targeted approaches) and consideration of genetic risk factors [2, 16]. Implementation of MRI-targeted biopsies in the screening procedure has been shown to reduce the number of biopsies among men with elevated PSA levels, increase the identification of clinically significant cancers (Gleason score ≥7) and reduce the number of insignificant cancers diagnosed [17–19]. The Swedish STHLM3-MRI study found that among men with a PSA ≥3 ng/ml, the detection rate of clinically significant cancer was similar among men randomised to either MRI or the Stockholm3 risk score (combination of protein markers, genetic polymorphisms and other clinical factors) [13]. This may indicate a better yield of MRI-enhanced screening than the Stockholm3 risk score. The Göteborg-2 study showed that adding the 4Kscore (a combination of kallikrein markers) as a reflex test to the screening algorithm could avoid 41% of MRIs, 28% of biopsies and 23% of low-grade cancer diagnoses. However, it remains unknown whether adding MRI-targeted biopsies reduces prostate cancer-specific mortality.
When to start and stop screening
Early start minimises the risk of missing cancer in younger men but may introduce unnecessary anxiety among men with a very low risk of dying of prostate cancer. Starting at an older age increases the risk of missing cancer and may increase the likelihood of men having a PSA test before enrollment in the screening programme. The recommendations of the first PSA test vary between current guidelines from 40-50 years, according to the European Association of Urology, to 55 years following the American Urological Association, with the latter being based on evidence from the ERSPC trial that starts screening at that age [3, 20, 21]. However, the Göteborg trial invited men aged 50 years and found a larger reduction in prostate cancer mortality than the ERSPC [10]. Analyses from the trial further showed that it is better to start screening at 55 than at 60 years [21]. Determining the optimal age to initiate screening is challenging, as the screening trials found differences in mortality reductions for the included age groups and study centres [8].
When considering the age when PSA-based screening should be initiated, factors like family history and ethnicity should be considered. Most guidelines recommend shared decision-making, which obliges doctors to discuss the benefits and harms of participation in systematic screening based on the individual’s health and expectations. Although easily written in the guidelines, this is not necessarily a straightforward task, especially not in a healthcare system that is pressed for time and trained staff. Shared decision-making may be even more complicated among men with low literacy, a low socioeconomic position and foreigners [22].
Determining when to stop systematic screening is also challenging. Prostate cancer incidence and mortality are strongly related to age, and most men dying from the disease are above 80 years [23, 24]. Screening of elderly men strongly increases the risk of overdiagnosis due to a higher likelihood of death from other causes. Unpublished data from the ERSPC showed that prostate cancer mortality was lower among men in the screening arm than in the control arm 12 years after stopping screening, but very low in both groups, questioning the importance of the mortality reduction (data presented at the European Association of Urology Annual Meeting, Madrid 2025).
PSA-testing outside screening programmes
PSA testing outside the screening programme may camouflage the true effect and inhibit the reduction in opportunistic PSA testing, which is neither beneficial for the male population nor for the healthcare system. In the Finnish ProScreen trial, 44% of the men (aged 50-67 years at invitation) randomised to screening had a PSA test before inclusion, most likely due to high age at invitation [25]. However, in the German PROBASE study, 34% had a rectal examination, and 16% had a PSA test before entry (age 45 years). Furthermore, 25% of men with delayed entry (PSA test at age 50 years) had a PSA test between enrollment and entry, which is in glaring contrast to the fact that almost 90% of the men with a PSA test at age 45 years were rated as low-risk (PSA ≤1.5 ng/ml), leading to a new PSA test after five years. This may indicate that awareness of prostate cancer and the possibility of early detection may cause men to seek PSA testing outside the screening programme.
Screening programme participation
A crucial factor for the success of systematic screening for any disease is a high participation rate. The ERSPC and the ProScreen trials have comparable participation rates (47% versus 51%), whereas only 12% of those invited participated in the PROBASE trial [15, 25, 26]. A low participation rate will decrease the observed effect in the general population and lower the true effect among men following the screening programme. In Denmark, screening programmes are currently running for breast, colorectal and cervical cancer, with participation rates around 84%, 60% and 62%, respectively [27]. Only for breast cancer, the rate met the pre-established standard. For colorectal cancer, a lower participation rate was found among men with younger age, short education and ethnic minority backgrounds. Achieving a satisfying participation rate for a prostate cancer screening programme in Denmark might therefore be challenging.
Long-term consequences of prostate-specific antigen testing
Treatment of low-risk prostate cancer detected by PSA-based screening is not without consequences. Complications and late effects are an inevitable consequence of cancer treatment, but while adverse outcomes may be considered acceptable when treatment leads to prolonged survival or symptom relief, this justification is often lacking in the context of low-risk prostate cancer, where many treatments have no such benefits. The most common late effects after treatment of low-risk prostate cancer are erectile dysfunction, urinary incontinence and bowel dysfunction, depending on the used procedure [28].
To reduce overtreatment, some men are offered active surveillance, where the cancer is monitored regularly to postpone active treatment. Active surveillance is equal to radical prostatectomy and radiation regarding prostate cancer-specific survival [29]. Five years after initiation, ~40% of the patients had received a radical intervention. Although active surveillance may reduce the harms of overdiagnosis, it does not prevent healthy men from becoming cancer patients.
Is it time to initiate systematic screening for prostate cancer in Denmark?
PSA-based screening reduces prostate cancer mortality, but the absolute effect on the number of deaths is limited. Based on ERSCP data, the expected reduction in Denmark is approximately 260 fewer annual deaths 20 years from now if PSA screening is introduced. Although new tools such as MRI, genetics and other concomitant biomarkers may reduce some of the harms associated with overdiagnosis, many unanswered questions remain in relation to the economic, societal and psychological burden imposed on the male population.
The PSA test is already widely used in Denmark, often in an unsystematic and inappropriate manner - for example, in men over 80 years, where benefits are limited, or in men with lower urinary tract symptoms, which are not associated with prostate cancer [30]. The Danish healthcare authorities have attempted to reduce the application of the PSA test by introducing National guidelines and information targeting men and general practitioners, but without noticeable effect. This fuels the debate about how we secure an optimal use of the PSA test – maybe even systematically – to avoid the harms of opportunistic screening. We need to carefully consider the next steps towards early prostate cancer detection. Systematic screening will neither eliminate prostate cancer mortality nor the treatment expenses of advanced disease. However, in a healthcare system under considerable pressure, we are obligated to limit superfluous tasks and expenses such as opportunistic PSA testing; not just to save money and personnel, but first and foremost to spare healthy men from avoidable harms, premature diagnosis and needless treatment.
We therefore urge Danish politicians to engage in the debate, as we are moving away from a scientific discussion towards an overall healthcare decision regarding a screening programme for prostate cancer in Denmark. Moreover, the interpretation and potential implementation of the EU Beating Cancer Plan call for debate in the healthcare policy system.
Correspondence Signe Benzon Larsen. E-mail: signe.liv.benzon.larsen@regionh.dk
Accepted 3 October 2025
Published 16 October 2025
Conflicts of interest AR reports financial support from or interest in William Nielsens Fond, Astellas A/S, Bayer A/S and AstraZeneca. All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. These are available together with the article at ugeskriftet.dk/DMJ.
References can be found with the article at ugeskriftet.dk/DMJ
Cite this as Dan Med J 2025;72(11):A09250711
doi 10.61409/A09250711
Open Access under Creative Commons License CC BY-NC-ND 4.0